Osteoarthritis is the most common form of arthritis that causes pain and inflammation in joints. It can affect almost any joint in our body, like knees, hips, hands, feet, and shoulder. Pain and joint stiffness are the main symptoms in OA that bring people to health care professionals. But little is known about what causes pain in OA.
Up to now, understanding of OA remains as a mechanical concept that the joint’s shock absorber or cushioning effect is worn away due to old age. This creates false beliefs that OA can be ‘fixed’ by replacing the worn structure in the joint. This also builds high hopes on passive treatment approaches like intake of supplements and stem cell injections.
A mechanistically biased approach to OA has created a dependency on imaging like X-ray/ MRI and treatments are decided mainly based on imaging results.
If pain in OA is due to lose of cushioning effect in the joint, people who had surgery for OA (for eg: knee replacement) should be pain-free post-surgery!! Shouldn’t they??
But we know that about 20 % of people are dissatisfied with the post-surgery outcomes. A significant proportion of people suffer ongoing knee pain despite having to go through risky surgical procedures.
The dissatisfaction is not because of failed treatment, but the treatment’s inability to meet the patient’s expectations. Concepts about diseases and illnesses are deeply rooted in society and the mechanical concept of OA is not an exception.
One study explored misconceptions about OA and participants expressed their understanding about OA in this study as ‘Wear and Tear’, ’Bone on bone’, ‘bald bones’, empty shells, ‘joint is beyond use by date’.
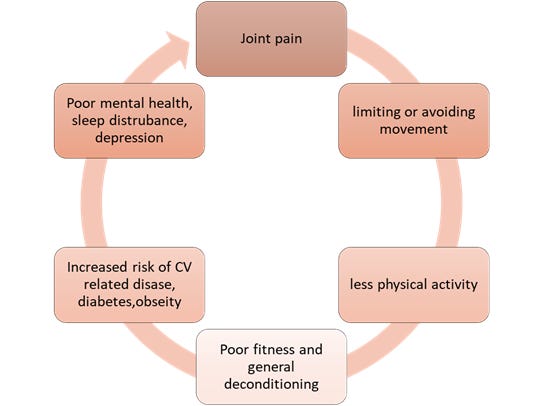
This outlook about OA probably creates a false association of its common clinical features such as cracking in the joint, sharp catching pain with weight-bearing, unsteadiness in joint, and transient stiffness to cartilage/ cushioning / lubricant loss. It is not uncommon for people with OA to lose trust in exercises and first-line medications. It is natural to avoid and protect the body part that hurts. This protective behavior deteriorates joint health in the long term leading to more diseases and disorders.
New evidence informs that osteoarthritis is not a passive process, otherwise, this cannot be compared to erosion or abrasion of mechanical parts in a car that can be replaced. It is a combination of peripheral-central mechanisms; that is, some usage-related changes in the joint, effects of repair process on joint structures, genetic factors, metabolic factors, immune system abnormalities, psychosocial contributors (mental health), and many more, all have a role in this active disease.
To simply put, it is not an isolated cartilage-related problem, butan issue of the whole joint as an organthat is influenced by multiple factors. It is more appropriate to address OA as an illness of a person rather than a disease of the cartilage.
It is an imbalance between joint injuries and the repair process
Joint replacement is most beneficial for people who are limited severely in their functions, inability to have a quality of life, and their personal safety is in jeopardy due to their joint problem, (eg: inability to walk between rooms within their home, difficulty to raise from a chair, inability to stand at one place for 5 mins, fall injuries due to joint unsteadiness, etc.,). Otherwise, what they call, end-stage osteoarthritis- a complete mechanical joint failure. (Grade 4 or 5 osteoarthritis as per Kellgren-Laweren scale).
If knee replacement surgery is not for everyone, what should others do for a better quality of life?
Research is being conducted to improve our understanding of OA pathology, who is at more risk of developing OA, who would respond better to what type of treatments, how should we better diagnose it, what is the best management for this disease, can we prevent this? Most of the studies are in infancy but we know
1. The older we get, the more risk for us developing osteoarthritis.
2. Female gender is more prone to develop OA than male
3. Increased Body Mass Index ( height/ weight )
4. Cumulative sprain or previous multiple joint injuries from heavy mechanical work or sporting injuries
5. Genetic factors – family history of OA
6. Severe joint deformities from birth for eg: hip dysplasia or knock knees
What controls do we have on the risk factors, how much can we influence a change?
BMI -Losing 10% of body weight will improve knee pain, systemic inflammation (pain-causing chemicals) health-related quality of life (reduce risk of heart disease, diabetes)
Be informed- educated better about this condition - Getting first-hand information from trusted websites like https://www.versusarthritis.org/
Emotions and mood- It is common to feel low and depressed or angry on ourselves due to arthritic pain. It is important to have a good frame of mind - mind and body are interlinked. So, having an optimistic outlook, simple self-management strategies, asking for help when needed, sharing emotions, and staying active we can manage this efficiently.
Lifestyle factors- sleep, diet, physical activity, work-life balance
Leg muscle weakness – Strength training and cardio exercise- walking programs, bodyweight exercises 15-30 mins a day x 4 -5 times a week.
Finally...
That’s all for now!! Thank you for your time. If you find this piece useful, please share it with your friends.







Easy to understand everyone...
Really a great read. Thanks for the informative article Mr.Yuvaraj.